Laser Cataract Surgery Combined With Premium IOL Implantation
In all cases, distance UCVA and BCVA improved to at least 20/30 postoperatively.
Aloysius Joseph Low, MBBS, FRCS
My introduction to femtosecond laser technology began in 2003, when we purchased an IntraLase (now Abbott Medical Optics Inc.) for our LASIK surgery center. Our practice quickly became known as a no-blade LASIK center. Seven years later, when we had an opportunity to purchase the LenSx femtosecond laser (Alcon Laboratories, Inc.), the idea of being also known as a no-blade cataract surgery center was enticing.
Instituting a new technology can be intimidating, especially when adding it to a procedure like cataract surgery, for which conventional phacoemulsification already provides excellent results in good hands. However, we strongly believe that femtosecond laser technology is the future of cataract surgery, similar to how the microkeratome has given way to femtosecond lasers in refractive surgery over the past decade.
OBSERVATIONAL STUDY
The first LenSx cataract surgery at Vista Eye Specialist was performed in October 2011, and to date we have completed 600 cases. An early observational study compared the visual outcome of 48 LenSx eyes with premium IOL implantation to 48 conventional (blade) phacoemulsification eyes with premium IOL implantation. All eyes were treated using the Infiniti Ozil IP Vision System (Alcon Laboratories, Inc.); in each group, 28 eyes were implanted with the AcrySof ReStor and 20 were implanted with the AcrySof ReStor Toric (Alcon Laboratories, Inc.). Exclusion criteria were concomitant ocular pathologies, hard brunescent cataracts, white intumescent cataracts, posterior polar cataracts, nondilating pupils or those that were difficult to dilate during the preoperative visit, small and tight palpebral fissures, and uncooperative patients.
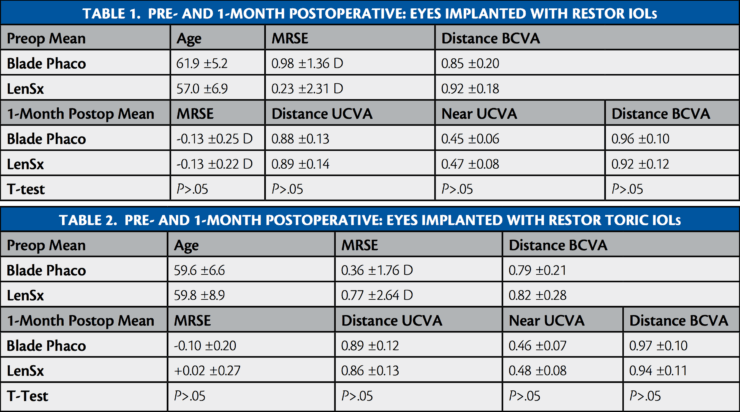
One-month postoperative results for eyes implanted with the ReStor IOL are found in Table 1, and 1-month results for eyes implanted with the ReStor Toric IOL are found in Table 2. In short, our results showed that the postoperative distance UCVA in both the LenSx and blade phaco eyes improved to 20/30 or better in the ReStor IOL group; 57% of the LenSx eyes and 54% of the blade phaco eyes achieved 20/20 distance UCVA (P>.05). Similarly, near UCVA in both groups improved to J2 or J3 at 1-month postoperative, with 50% of the LenSx eyes and 57% of the blade phaco eyes achieving J1 (P>.05). Across groups implanted with the ReStor IOL, all eyes achieved a cumulative distance BCVA of 20/30 or better, with 82% of LenSx eyes and 86% of blade phaco eyes achieving 20/20 (P>.05).
In the ReStor Toric IOL groups, 45% of LenSx eyes and 50% of blade phaco eyes achieved 20/20 distance UCVA (P>.05); 45% of LenSx eyes and 55% of blade phaco eyes achieved a cumulative near UCVA of J1 (P>.05); and 85% of eyes in both groups achieved 20/20 cumulative distance BCVA (P>.05).
LESSONS LEARNED
A video demonstration of my laser cataract surgery technique is available at eyetube.net/?v=michi. Additionally, below are seven lessons I have learned using the LenSx femtosecond laser for cataract surgery.
Lesson No. 1: Always try to center the eye well. If it is difficult to center an eye during docking, make sure the eye is well-centered around the limbus before pressing the accept button. This may prevent nonuniform laser energy distribution during the capsulotomy and a resultant radial tear of the anterior capsule.
Lesson No. 2: Some pupils constrict immediately after the laser is applied. Therefore, be prepared to use 0.25 mL of intracameral preservative-free phenylephrine HCl 10% intraoperatively.
Lesson No. 3: It may be wise to mark the peripheral cornea at the site of the intended corneal incisions. This strategy helps to ensure that the laser will cut the cornea only, and not the conjunctiva or blood vessels, which makes it difficult or impossible to open the incisions. In such difficult cases, the surgeon may have to resort to using a blade. Usually the corneal incisions open with the Slade Femtosecond Spatula (ASICO, LLC) or Seibel Spatula (Rhein Medical).
Lesson No. 4: Always stain the anterior capsule with trypan blue before attempting to remove the anterior capsule. I remove the anterior capsule in laser cataract surgery cases the same way as in my conventional phaco technique. This ensures that all capsular microtags are properly broken with good control.
Lesson No 5: Only gentle hydrodissection is needed. If the surgeon slightly depresses the nucleus and a lot of air bubbles are seen escaping from behind the nucleus toward the anterior chamber, there may be no need for hydrodissection. In these cases, the nucleus will rotate with ease.
Lesson No. 6: During cortex removal, there are no cortical strands to help in the removal, as are found in conventional phaco. This is because, during the capsulotomy, the laser also cuts the underlying cortex flush with the anterior capsular edge. It is easier to sweep tangentially below the capsular edge and thereby aspirate a broader leaf of cortex.
Lesson No. 7: A longer postoperative follow-up is beneficial. Because this technology for cataract surgery is still in its early stage, following patients for up to 6 months is perhaps crucial.








































