As For Now
By Lim Boon Siong
Since the time of the launch of LACS at Vista Eye Specialist in October 2011, much has changed in the cataract surgery landscape, from the increased number of femtosecond laser cataract platforms in the market to the introduction of improved premium IOLs. These changes, along with some successes and challenges that arose, required us to continually refine our marketing strategies for offering modern cataract surgery, which includes LACS.
Our conversion rate to LACS stands currently at about 58%. However, the number of cases performed so far in the past 5 years remain low with only 2,500-plus cases. Below I share three successes and challenges associated with LACS.
Success No. 1: Higher patient satisfaction, faster healing. One of the keys to our success has been a high level of patient satisfaction, as evidenced by high referral rates to patients’ relatives and friends. We have also seen higher patient satisfaction with LACS in our patient surveys compared with traditional phaco surgery, and our surgeons report increased positive patient feedback, especially from those who had the traditional procedure in the first eye. The surgeons also report better clinical results, particularly in cases in which premium IOLs are implanted. Noticeably, we have also seen that patients are generally happier on postoperative day 1 due to faster healing.
Success No. 2: More surgeon confidence in offering refractive lens exchange (RLE).Along with these successes in cataract surgery, our doctors have become more confident in offering RLE for patients in their 40s and 50s who are frustrated with their presbyopia symptoms. Hence, we have seen a surge in conversions of both LACS and premium IOL selection for this group of patients.
Success No. 3: Raising the profile of the practice. The introduction of LACS has helped to raise Vista’s branding and profile in the local and international ophthalmology fields, and it has enhanced our reputation and perceived image among our patients that Vista is the most technologically advanced practice in our region.
Challenge No. 1: Creating awareness and communicating the benefit. With any new product introduction, the challenge as we move past the introductory stage is to continue to fine-tune and improve our communication about the product. Despite producing a series of materials, advertising, and promotional activities, the biggest challenge remains trying to create awareness of our LACS technology and to communicate the benefits in ways that patients can understand. We also face the challenge of disbelief in our technology among other practitioners who do not offer LACS.
Challenge No. 2: High pricing. The other challenge to ultimately becoming a 100% LACS center remains the pricing strategy. The difficulty lies in finding an optimum price that is affordable to patients yet that yields a healthy return to the practice. With the high capital investment and disposable costs, the premium price of an add-on of US$950 per eye on top of our traditional cataract fee remains beyond the reach of most patients. This is further complicated by the perceived marginal benefit of LACS over traditional cataract surgery in terms of results and safety.
Pricing remains the biggest barrier to success with LACS. The key reasons LACS has not been an instant success come down to high cost and low patient awareness. We need to have a long-term plan, along with strong perseverance and stamina in execution, to increase awareness and the adoption of this new technology into our practice. Unless we find a secret formula to lower prices to a more affordable level (by at least 50%), this life-changing technology will remain exclusive to only a privileged, small segment of the market.
ORIGINAL ARTICLE: OCTOBER 2012
Laser Cataract Surgery Combined With Premium IOL Implantation
By Aloysius Joseph Low, MBBS, FRCS
AS OF NOW
Lessons Learned with LACS
Vista Eye Specialist is known in Malaysia as the No-Blade LASIK and Cataract Centre. We introduced femtosecond laser technology in 2003 for LASIK and in 2011 for LACS. Our experience with femtosecond lasers includes the IntraLase (Abbott), Lensar Laser System (Lensar), and LenSx (Alcon) devices, and we are in the process of reviewing other femtosecond lasers for LACS.
OBSERVATIONAL STUDY
To update my article from 2012, I here compare the visual outcomes of 50 eyes undergoing LACS with the LenSx laser system and implanted with Lentis Mplus X nontoric IOLs (Oculentis) versus another 50 eyes implanted with the same type of IOL using blade incisions and conventional phacoemulsification with the Infiniti Vision System with Ozil Intelligent Phaco (Alcon). Exclusion criteria were concomitant ocular pathologies, hard brunescent cataracts, white intumescent cataracts, posterior polar cataracts, pupils that were nondilating or were difficult to dilate during a preoperative visit, small and tight palpebral fissures, and uncooperative patients.
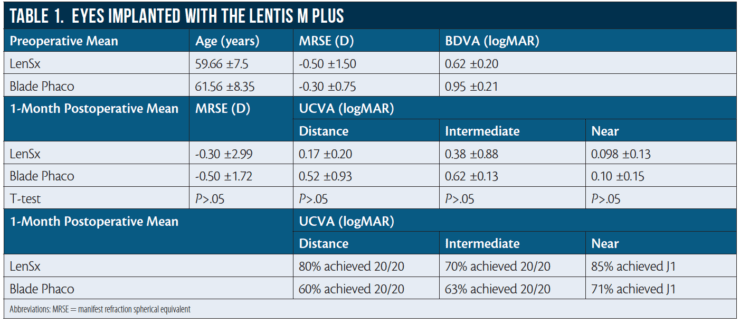
Preoperative data and 1-month postoperative results for eyes implanted with the Lentis Mplus X are shown in Table 1.
In the LenSx group, at 1 month postoperative, mean UDVA was 0.17 ±0.20 logMAR and 80% (40 eyes) achieved 20/20; mean UIVA was 0.38 ±0.88 logMAR and 70% (35 eyes) achieved 20/20; and mean UNVA was 0.09 ±0.13 logMAR and 85% (42 eyes) achieved J1 (N3). In the blade/phaco group, mean UDVA was 0.52 ±0.93 logMAR and 60% (30 eyes) achieved 20/20; mean UIVA was 0.62 ±0.13 logMAR and 63% (31 eyes) achieved 20/20; and mean UNVA was 0.10 ±0.15 logMAR and 85% (42 eyes) achieved J1 (N3).
LESSONS LEARNED OVER 5 YEARS
Lesson No. 1: When to redock. The autocentration of the LenSx does a good job, but, sometimes, the surgeon may want better centration. In this case, it is best to redock. Do not at any time at this stage attempt centration with the joystick.
After autocentration and docking have been done, if the surgeon notices an air bubble or corneal fold under the area to be lasered, again, redock. Do not proceed with the laser before redocking, as this may result in nonuniform laser energy distribution during capsulotomy and a resulting radial tear of the anterior capsule.
Lesson No. 2: Pupil constriction. Some pupils constrict immediately after the laser is applied. Nowadays, we place a small cotton pledget soaked in 2.5% phenylephrine and 1% tropicamide into the inferior fornix while the patient is in the dilation room. Additionally, we are prepared to inject 0.25 mg of intracameral preservative-free phenylephrine 10% intraoperatively.
Lesson No. 3: Marking the eye. Using a surgical marking pen, mark the peripheral cornea at the 3- and 9-o’clock positions and at the site of the intended corneal incision. This not only facilitates the placement of toric IOLs but also prevents the laser from cutting the cornea too centrally.
Lesson No. 4: Staining the eye. Intraoperatively, do not hesitate to use trypan blue dye to stain the corneal incisions and the anterior capsule. Some corneal incisions may be difficult to visualize due to microscopic air bubbles in the vicinity. Most anterior capsules float easily, but if you are in doubt of the presence of capsular microtags, the trypan blue stain will help to ensure that microtags can be properly broken with good control using capsulorrhexis forceps.
Lesson No. 5: What now? Is LACS dying a natural death? In these 5 years, we have done only 2,500-plus LACS cases, despite adequate marketing efforts. This is far from enough volume. There is a need for changes in the mindset of cataract surgeons still reluctant to adopt this technology. Industry players should accept that high pricing is the biggest barrier to greater adoption of this technology and play their role by bringing down the cost of this technology to make it as affordable as possible for patients.
